Expanding Orthopaedic Access




New Orthopaedic Residency Will Expand Access, Train Surgeons for El Paso, in El Paso
The program will keep up to 15 medical residents in El Paso by 2030, enhancing and delivering faster musculoskeletal care across our Borderplex
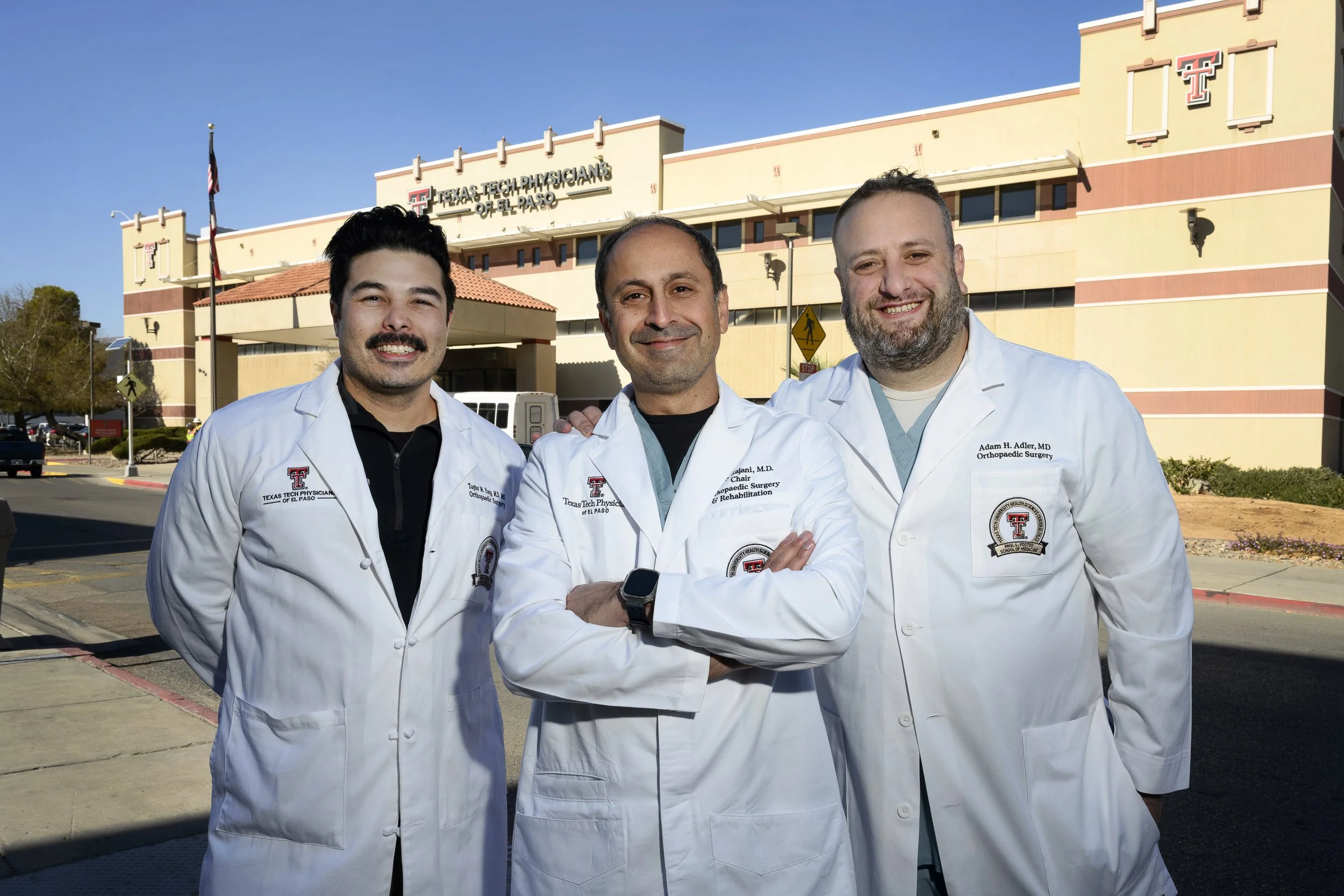
Saturday nights can be busy for Texas Physicians of El Paso doctors working in the trauma bays at University Medical Center of El Paso. EMTs wheel in patients who have experienced severe falls, car accidents resulting in complex fractures, or they might have serious conditions like bone cancer. What many of them share is their wait to see an orthopaedic specialist like Rajiv Rajani, M.D.
Starting July 1, 2026, a new orthopaedic surgery residency at Texas Tech Health El Paso will provide Dr. Rajani, who chairs the university’s orthopaedic surgery program, with the first of up to 15 more hands and eyes on the front lines of care right here in our Borderplex. For families across the region, that means faster care when every minute counts.
By training three residents each year in a five-year program at UMC, the university’s primary academic hospital, Texas Tech Health El Paso aims to increase the number of orthopedic surgeons and expand subspecialty care. The program also aims to increase the likelihood that graduates will stay and practice in El Paso and nearby communities. For patients, this means more orthopedic specialists available in exam and operating rooms here at home, and the ability to accommodate more patients with complex surgeries that previously required travel or long delays.
“Residency is your pathway for local care,” said Dr. Rajani, who will also direct the new residency program. “When you talk about musculoskeletal health, El Paso is underserved. Training here helps us build, retain and stabilize high-quality orthopaedic services for our community.”
The program aims to train up to 15 individuals by 2030 to fill a documented gap in orthopaedic surgeons.
“This is a major achievement for families across West Texas and Southern New Mexico," said Armando Meza, M.D., associate dean of the university’s Graduate Medical Education program. “It broadens our institution’s postgraduate training options and supports efforts to address the physician shortage in our region."
When Dr. Rajani describes the orthopaedic caseload in El Paso, the numbers tell a story: Specialist care has struggled to keep pace with population growth.
Orthopaedic residents who join the new program will gain experience as unique as our Borderplex. Unlike programs that rotate residents across multiple cities, this program keeps the full training pathway here.
Core rotations anchor within the El Paso region at UMC, the area's Level I trauma center, with educational partnerships across academic hospitals and community practices.
The program is distinct from — yet collaborative with — the long-standing combined program at William Beaumont Army Medical Center, which has trained five orthopaedic residents per class with one civilian slot. “We’re transitioning from a shared program to our own civilian residency,” Dr. Rajani said. “The responsibility is ours to do it well.”
An orthopaedic residency transforms a newly graduated medical student into a practicing surgeon. Each first-year doctor perfects histories, physical exams, musculoskeletal assessments, suturing and wound care. As they progress, the resident takes on independent roles in basic procedures, and handles complex cases under the supervision of attending physicians.
For Natalie Devitto, a third-year medical student at the Foster School of Medicine from Dallas with roots in El Paso, she hopes to join the program upon graduation.
“It’s very exciting and I think opens a lot of opportunities for students like me,” said Devitto. “If you train in El Paso, then you are likely to stay in El Paso.”
The layered training unfolds against a backdrop few single-city programs can offer. El Paso's binational footprint produces a broad case mix, with patients needing care in trauma, oncology, sports medicine, spine, hand surgery, foot and ankle, and pediatrics.
“We see everything here,” Dr. Rajani said. “The combination of a Level I trauma center, border-related trauma, oncology and a vast service region creates uncommon training depth.”
Quality underlies every decision. “Academic hospitals deliver better outcomes because someone is in the hospital who can evaluate patients almost 24/7 when issues arise,” Dr. Rajani said. The department manages approximately 20,000 patient visits annually. To support education and demand for services, the department plans to grow faculty numbers from 10 to 14.
Interest in the new program, which starts in the summer of 2026, is already strong. The program has received nearly 200 applications for three positions. “There's no expectation we'll have unfilled spots,” Dr. Rajani said.
For El Pasoans wondering what will change July 1, when the new orthopaedic residents begin at UMC, the most immediate difference is in time and attention: more hands for evaluations, more eyes on complex cases and deeper follow-up coordination. The longer-term difference is in continuity — the likelihood that doctors who train here will stay here, strengthening a stable musculoskeletal-care network for our Borderplex.
About Texas Tech Health El Paso
Texas Tech Health El Paso serves 108 counties in West Texas and is dedicated to preparing the next generation of health care heroes. Established as an independent university in 2013, Texas Tech Health El Paso is a uniquely innovative destination for medical, nursing, biomedical sciences and dental education.
Focusing on excellence in health care education, research, and clinical service, Texas Tech Health El Paso has graduated over 2,600 professionals over the past decade. For more information, visit ttuhscepimpact.org.
